together,
we have the power to take onTK2d
If you're just learning about thymidine kinase 2 deficiency (TK2d) or suspect you may have TK2d, genetic testing is the most accurate way to diagnose TK2d and can help people get the care they need sooner.

If you're just learning about thymidine kinase 2 deficiency (TK2d) or suspect you may have TK2d, genetic testing is the most accurate way to diagnose TK2d and can help people get the care they need sooner.
What is TK2d?
TK2d is a rare genetic mitochondrial disease
Mitochondrial diseases are a group of rare, debilitating, and often fatal conditions with a severe impact on daily living and quality of life. TK2d is a type of mitochondrial disease called mitochondrial DNA depletion and deletion syndrome (MDDS).
There are many types of mitochondrial diseases, so while they are rare, it is estimated that 1 in every 5,000 people is affected.
Watch this quick video to get a better understanding of the cause of TK2d, as well as symptoms, treatment, and other important facts.
To best understand mitochondrial diseases like TK2d, there are some things about the body that you need to know first.
Mitochondria and ATP


Inside almost all human cells are mitochondria, the powerhouse of the cell. Their job is to make the energy that is essential to many critical body functions, like the beating of your heart. This energy is called adenosine triphosphate, or ATP.
DNA and mtDNA


You may know that some DNA is stored inside the nucleus of your cells (called nuclear DNA), but did you know that we also have mitochondrial DNA (mtDNA)? This mtDNA plays an important role in creating ATP.
Mitochondrial disorders


To make ATP, the mitochondria need enzymes and other proteins from both nuclear DNA and mtDNA. When there is an error (mutation) in either type of DNA, it can cause a mitochondrial disorder.
Understanding TK2d
TK2d is a primary mitochondrial myopathy, which means that it affects muscles. It is also a type of mitochondrial disease called mtDNA depletion/deletion syndrome.
Thymidine kinase 2 (TK2) is an enzyme that helps make and maintain your mtDNA. When you have a healthy and normal amount of mtDNA, the mitochondria are able to create and provide energy for your body and its functions.
What causes TK2d?
TK2d is caused by mutations in the TK2 gene, which decrease the enzyme activity that helps make and repair your mtDNA. Because there isn't enough healthy mtDNA, the mitochondria cannot work the way they should. This means muscles don't have enough energy and cannot function properly. This can lead to weakness in many muscle groups.
quick facts
TK2d can develop at any point in life. It's considered early onset if symptoms appear at or before 12 years of age, and late onset if they develop after. If symptoms began before 12 years but you were not diagnosed until adulthood, this is still early-onset TK2d.
- TK2d was first described in children in 2001
- In 2013, improved genetic testing led to the discovery of an adult-onset form of TK2d
- TK2d shares symptoms with many other diseases, so there may be people living with TK2d who have not been diagnosed
- Genetic testing can provide an accurate TK2d diagnosis
If you suspect TK2d, ask your doctor about confirming a diagnosis with genetic testing. If you have already had a genetic test, ask your doctor if TK2d was included on the testing panel. If it wasn't, consider testing again.
What are the symptoms of TK2d?
TK2d has progressively taken away my physical strength, my ability to eat, swallow, and breathe.
What are the symptoms of TK2d?
TK2d causes a spectrum of symptoms that can impact people of all ages
TK2d is defined by weakness in the muscles (called myopathy) closest to the center of the body. It can affect life in a range of ways. Many people with TK2d lose the ability to walk, eat, and breathe independently. Tragically, it is life-threatening.
Symptoms can progress slowly or quickly, depending on the person and age of onset. Generally, the earlier in life symptoms start, the quicker they progress and become life-threatening.
Because TK2d is a disease with many symptoms, diagnosing TK2d can be a long journey. Patients may be misdiagnosed with other conditions, such as spinal muscular atrophy (SMA) or muscular dystrophy. If you suspect TK2d, talk to your doctor.
Symptoms of
Early-onset
TK2d
Many people whose symptoms began at or before age 12 had a healthy birth and reached early developmental milestones. Shortly after, they may have experienced:

Many people whose symptoms began at or before age 12 had a healthy birth and reached early developmental milestones. Shortly after, they may have experienced:
(trouble breathing)
Difficulty swallowing
(loss of the ability to sit and hold their head up, also called floppy baby syndrome)
(difficulty with and/or loss of skills like crawling, walking, balancing, and grabbing)
Symptoms of
Late-onset
TK2d
People whose symptoms began after age 12 often have symptoms that do not progress as quickly as early-onset TK2d, including:

People whose symptoms began after age 12 often have symptoms that do not progress as quickly as early-onset TK2d, including:
(progressive external ophthalmoplegia)
It is possible that a person first experiences symptoms as an infant or child, but does not get diagnosed until after age 12. This is still considered early-onset TK2d.
download and
share
A helpful resource for the TK2d community
Download to learn more about the cause of TK2d, symptoms, diagnosis, disease management, a multidisciplinary healthcare team approach, and patient community organizations and resources.
For me to be diagnosed took 21 years, probably due to lack of information about the symptoms and course of TK2d.
If you suspect TK2d, use genetic testing to confirm a diagnosis
If you or a loved one has several of the symptoms listed above and you suspect TK2d, talk to your doctor about genetic testing for TK2d. All you need to provide is a blood sample, a saliva sample, or a cheek swab, and there are several no-cost genetic testing options available.How is TK2d inherited?
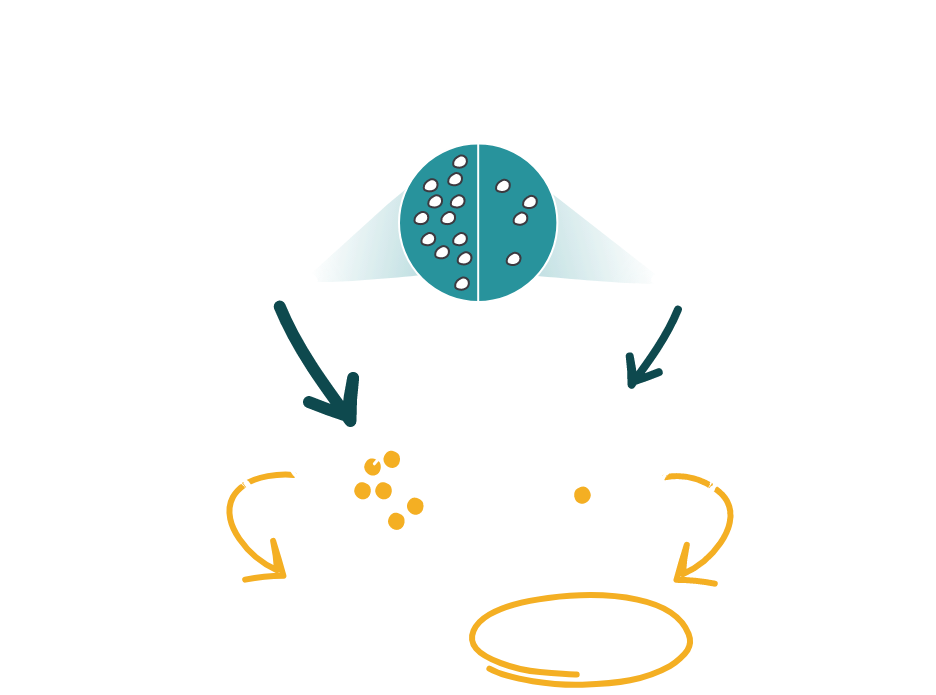
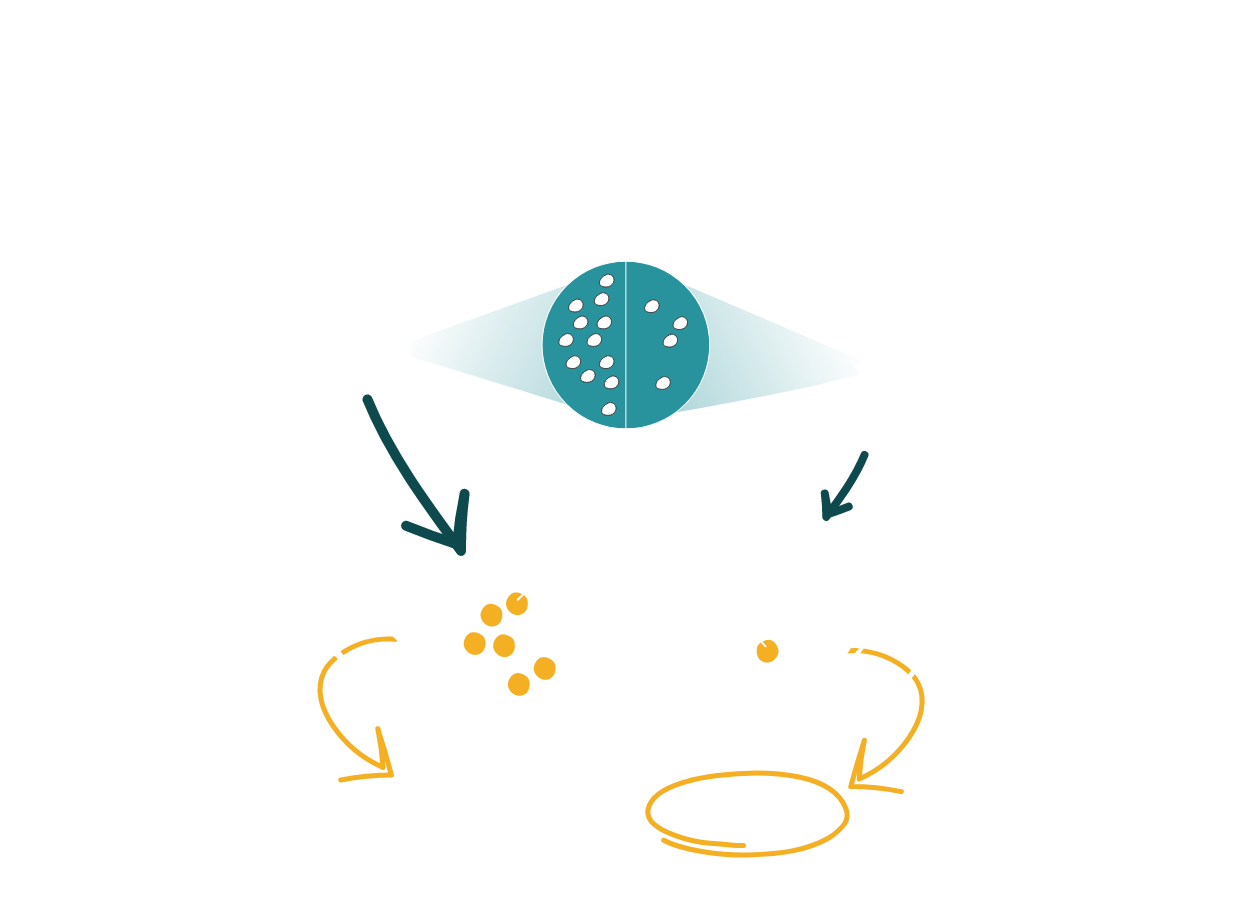
TK2d is an inherited mitochondrial disease caused by a genetic mutation in the TK2 gene. Both the mother and father (called carriers ) must have the altered TK2 gene for a child to get TK2d. This is called an autosomal recessive inheritance pattern.
When both parents are carriers of the TK2 gene, each child will have a 25% chance of having TK2d, a 50% chance of being an unaffected carrier, and a 25% chance of not having TK2d and not being a carrier.
The mother and father who pass on TK2d will usually not have any signs or symptoms of the disease. That is one reason why getting a diagnosis can be hard for someone who inherits TK2d.
If you or a loved one has been diagnosed with TK2d, you should also talk to your doctor about how to learn if siblings or other family members may be carriers.
TK2d inheritance:


TK2d inheritance:
These are the possibilities with two carrier parents:

25%
Chance of having TK2d
50%
Chance of being an unaffected carrier of a single mutated TK2 gene
25%
Chance of not having TK2dand not being a carrier
How is TK2d managed?
The first step to proper management of TK2d is getting the right diagnosis with genetic testing. TK2d can often have serious or life-threatening consequences, but once TK2d is confirmed, there are several ways healthcare providers can help manage the symptoms, try to slow disease progression, and limit its impact. They may use medical equipment and therapies such as:
- Respiratory support/therapy
- Feeding tubes
- Wheelchairs
- Physical therapy
- Nutraceuticals (sometimes called a mito cocktail)
Caring for someone with TK2d usually involves a multidisciplinary team that includes a physical therapist to help keep muscles functioning and other specialists as needed (eg, a pulmonologist to manage breathing problems). A multidisciplinary team may include:
- Neurologists
- Pulmonologists
- Metabolic specialists
- Gastroenterologists
- Pediatricians or primary care physicians
- Nutritionists
- Orthopedic specialists
- Occupational therapists
- Physical therapists
- Speech therapists
- Clinical geneticists
- Genetic counselors
While there are no FDA-approved therapies to treat TK2d, we continue to learn more about the disease and potential treatments
Sign up and stay informed
Because there is so much we do not know about TK2d, please help us grow the community so that our collective experience can be the driving force behind change. Register to stay on top of the latest developments and get updated about newsworthy milestones.*All fields are required.
In addition, all of our future communications will include an opportunity to opt out. WHO WE ARE Click here to learn more about UCB and our efforts to take on TK2d.

